By Dr. Carol Hoban
Faculty Member, School of Health Sciences
Obesity rates in children have continued to rise in the United States with the prevalence of obesity being almost 20% during 2017-2020 for children and adolescents. Commonly, a measurement called the Body Mass Index (BMI) is used to calculate someone’s obesity. It is calculated by dividing a person’s weight (in kilograms) by the square of that person’s height in meters.
The Difference between BMI and BMI-for-Age
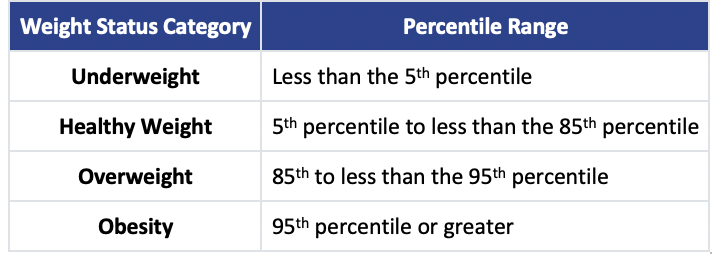
Because children are constantly growing and there is a difference between the BMI of girls and boys, their BMI is usually described as the BMI-for-age. The Centers for Disease Control and Prevention uses this chart to define the size and growth patterns for kids and teens with the BMI-for-age corresponding to percentiles within these categories.
The CDC also provides a calculator for assessing the BMI percentile for your child or teenager.
Over the last four decades, children have grown heavier and heavier, despite efforts to educate children and families on healthy nutrition and the importance of physical activity. Sadly, obesity rates are even higher among some ethnic groups, who may often rely on cheaper, less nutritious foods and who may not have a safe place for exercising.
Related link: Finding the Drive to Build New Post-Pandemic Healthy Habits
Being Overweight Impacts a Child’s Physical and Mental Health
Being overweight impacts not only the physiological health of children, but also their psychological health. The obesity epidemic amongst children today is a leading public health concern, and many studies have been conducted to understand the associations and risk factors of childhood obesity.
Studies examining obesity rates have shown that those rates are correlated with socioeconomic status (SES). In a study published by the CDC, researchers found that as the level of education or income of a child’s parents went up, obesity rates were lower. Other risk factors noted in several studies included family characteristics (the mother’s BMI or age at delivery) and childhood lifestyle (time spent watching TV, duration of sleep, and dietary habits).
Technology has certainly not helped with obesity rates. For instance, technological advances have contributed to more mass food production. In addition, kids have more screen time now than outside play time with the availability of smartphones and gaming websites.
Related link: 5 Habits to Improve Your Physical and Mental Health
Controlling Children’s Nutrition and Exercise to Reduce Obesity Rates
There are many factors that contribute to childhood obesity rates, including genetics, diet and a lack of exercise. While there are some physical factors that we cannot control (like our genes), we can try to modify children’s nutrition and physical activity.
Teaching children and teens about the food they eat, preparing healthy snacks such as fruits and veggies, and encouraging kids to get outside and play are all useful ways to combat childhood obesity. The U.S. Department of Agriculture has resources on teaching children to eat healthy meals, and there are even apps that can be downloaded to your phone or computer for additional tips on nutrition.
Summer Is a Great Time to Encourage Children and Teens to Get Exercise
Summer officially began in the U.S. on June 21, and now is the perfect time for kids of all ages to get outside and enjoy the weather. There are numerous physical activities for children and their families to enjoy, including swimming, hiking, walking and bike riding.
As the weather continues to heat up, summer is also the ideal time to enjoy the various fruits and vegetables popping up at local farmers’ markets all over the country. After all, what is better than enjoying a slice of cool, fresh watermelon after a nice bike ride on a hot summer day?

Comments are closed.